By Roxanne Lee
Staff Writer
Recent discoveries have highlighted the use of the parasite hookworm in treating autoimmune disorders, though the true subject of the research is not the parasite, but the molecules it produces.
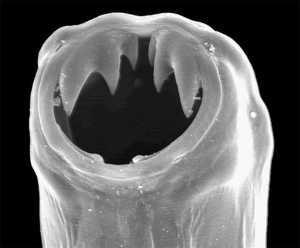
It is understandable that using hookworms as treatment in medicine is strange. Hookworms are parasitic nematode worms that infest the small intestines of birds and mammals. Two species in particular infest humans: Anclyostoma duodenale and Necator americanus.
Hookworms attach to the wall of the intestine to drink their hosts’ blood. If it is a light infestation, as most people who have the infection, there will not be any external symptoms. However, a heavy infestation can cause nausea, anemia, cramping, weight loss, abdominal pain, and protein loss.
There are 760 million hookworm infections worldwide and 25 million in the United States, though it used to be more widespread than that.
Their use in medicine comes in part from the hygiene hypothesis, which posits that the lack of exposure to germs and parasites in childhood leaves humans prone to develop more allergies and autoimmune disorders as they mature.
Scientists working at James Cook University in Australia studied the possible link between the decline in parasites due to improved public health and the rise of autoimmune disorders. They, as well as other teams of scientists, have used the parasite in studies of the treatment of autoimmune disorders such as inflammatory bowel disorder and Crohn’s disease, and have repeatedly found that the worms alleviate some of the symptoms. This suggests that diseases became more common as people became less infected with hookworms.
There is an understandable lack of appeal to the idea of purposefully being infested with intestinal parasites, so researchers at James Cook University found a solution that gets the best of the parasites without infecting anyone.
Immunologist Dr. Severine Navarro, co-author of the study, and her colleagues looked for a specific molecule responsible for the effects caused by parasites. To find it, they crushed and made “soup” from them. Of the 100 proteins found in the soup, one of most abundant was anti-inflammatory protein-2, AIP-2, that Hookworms secreted while attached in the gut that bolstered the immune systems of their hosts.
Researchers synthesized AIP-2 separately from the parasite and injected it into mice with asthma, then put mice through range of tests. They found that in the mice with asthma, AIP-2 suppressed airway inflammation. The AIP-2 shifted the balance of immune cells and shifted immune reaction in lung, and stopped high proliferation of T cells in the blood. The protein also changed immune cells in human skin when tested on skin samples of people with dust mite allergy. AIP-2 lessened production of dendritic cells and T cells, signs of a reduced allergy response.
Their eventual goal is to create synthetic versions of a drug to artificially replicate the effects of hookworm on autoimmune disorders. By doing this they would not have to purposefully infect people with the hookworm to get the benefits.
Researchers are in the process of isolating and testing more proteins from the soup, in the hopes of finding more that specifically affect autoimmune disorders,and Navarro and colleagues are now looking for a company to support a clinical trial.

















John • Nov 3, 2016 at 12:52 am
Even if and when helminth-derived drugs become available, these are unlikely to deliver the extent and quality of immune modulation that live worms are capable of and, like most other single molecule drugs, they will almost certainly produce significant long term adverse side effects, which small numbers of helminths don’t do.
“The learned thinking pattern for medical professionals and biomedical researchers is to envision isolation and characterization of the individual components produced by helminths, with the goal of creating new helminth-inspired drugs to treat disease. On the one hand, this approach is consistent with the general practice of modern medicine and the common approach used to find new drugs today. On the other hand, recapitulating the effects of an integral member or members of the biome using a single or even a handful of pharmaceuticals may prove extremely difficult. Indeed, given the complex and continuous nature of the interactions between host and helminth that have evolved over hundreds of millions of years, the design of therapeutics to entirely and effectively recapitulate this interaction may prove impossible.”
http://evmedreview.com/?p=457
“Helminth-derived pharmaceuticals might offer an alternative to biome reconstitution, but given what is already known about the complex and multi-faceted nature of helminth–host interactions, pharmaceuticals which effectively mimic the effects of helminths might prove extremely difficult and expensive to develop and utilize. Further, the low costs, high efficacy, and very low rate of side effects that are expected to be associated with biome reconstitution make this approach extremely appealing.”
http://www.ncbi.nlm.nih.gov/pubmed/21741180
“When you give someone a live worm, it’s like giving them the factory that makes the products and letting the factory do what it needs to do… Evolution has already created this thing.” (David Elliott, University of Iowa.)
“Twenty years from now everybody is going to have a helminth, and no insurance company will begin to cover you if you don’t have your helminths … We’re very confident in the science, that every single human being needs a helminth. It’s part of our biology.” (William Parker, Duke University, 2016)
http://pamplinmedia.com/pt/9-news/302838-180108-hooked-on-hookworms-and-other-parasites